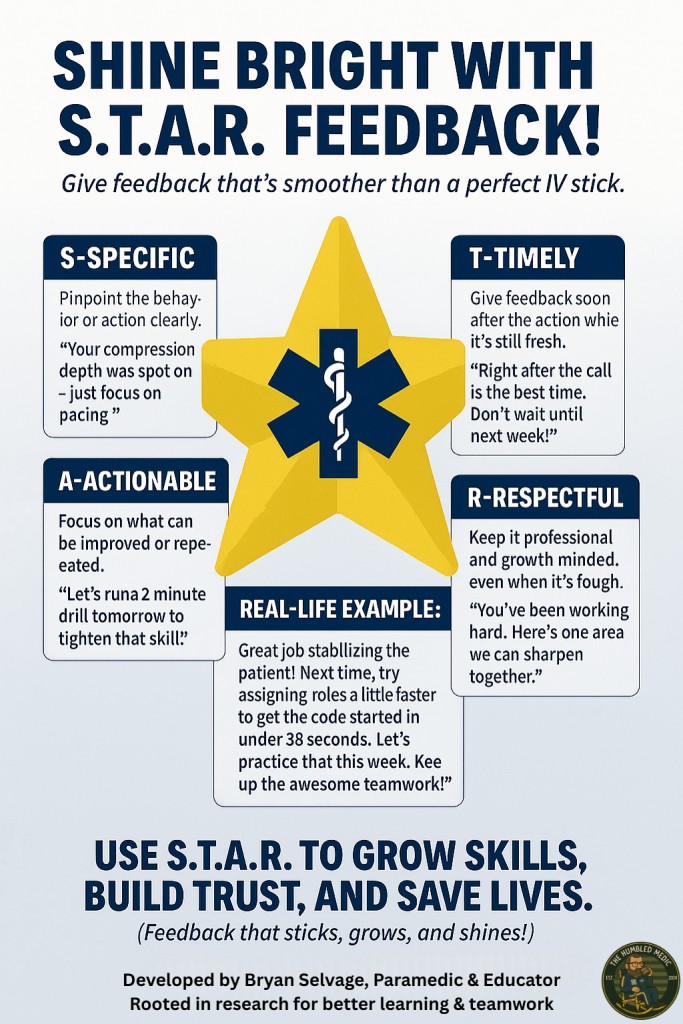
Let’s talk feedback—the secret sauce that keeps us sharp in this wild, high-stakes world of saving lives. It’s the nudge that turns a shaky IV stick into a work of art, the hint that makes a lecture less “snooze-fest” and more “standing ovation,” and the trust-building moment that keeps providers in sync. Done right, feedback is like a perfectly timed defibrillation: it shocks us into growth. Done wrong, it’s a fumbled IO attempt—painful and messy. As a paramedic with 20 years of calls under my bunker gear and an educator who’s been humbled by students and coffee spills alike, I’ve learned feedback is both science and soul. Today, we’re diving deep into the S.T.A.R. method (Specific, Timely, Actionable, Respectful), unpacking why each piece is critical, where and when to deliver it, and how to make it stick. Expect evidence-based wisdom, good and bad examples, new ideas, and a sprinkle of humor—because if I can’t laugh at my coffee stains, what’s the point? Grab your spill-proof mug, and let’s roll!
Why Feedback Matters: The Evidence-Based Backbone
Feedback isn’t just a pat on the back or a kick in the shins—it’s how we grow in EMS and nursing, where precision can mean life or death. A 2019 meta-analysis by Wisniewski et al. in Medical Education found that well-crafted feedback boosts clinical performance by up to 25%. Hattie and Timperley’s 2007 study in Review of Educational Research nails it: feedback shines when it targets the task (e.g., “Your compression depth is solid”), the process (e.g., “Try pacing your assessment”), or self-regulation (e.g., “Reflect on your priorities”). Vague praise or harsh jabs? They’re as useful as a broken laryngoscope.
- Teacher to Student: Feedback bridges the gap from “I’m lost” to “I’ve got this.” When I tell a student their trauma assessment missed a key injury, I’m not dunking on them—I’m paving their path to mastery.
- Student to Teacher: Students keep us educators honest. I once had a student call my scenarios “more tangled than a soap opera.” They were right, and it forced me to rethink my game.
- Provider to Provider: This is where teamwork thrives. When a nurse nudges me to double-check a med dose (math’s not my jam), it’s not shade—it’s trust.
But feedback flops without the right approach, timing, or setting. Let’s unpack the S.T.A.R. method, dive deep into why each component is critical, and explore how to deliver it like a pro.
The S.T.A.R. Method: A Deep Dive into Each Component
I’ve seen feedback crash harder than a rookie driver in a snowstorm—like the time a preceptor shouted, “You’re too slow!” in a packed ED. Not cool. To avoid that chaos, I created the S.T.A.R. method (Specific, Timely, Actionable, Respectful), grounded in evidence and my own scars as an educator. Below, I’ll break down each piece, explain why it’s a game-changer, and tie it to EMS/nursing realities.
1. Specific: The Laser-Focused Foundation
- What It Means: Specific feedback pinpoints the exact behavior, skill, or decision you’re addressing. Instead of “You need to improve,” say, “Your compression depth was great, but you paused too long between cycles.”
- Why It’s Critical: Vague feedback is like telling someone to “fix” a seizing patient without naming the drug. It leaves the receiver confused and directionless. Specificity clarifies what’s working and what’s not, making improvement tangible. Kluger and DeNisi’s 1996 meta-analysis in Psychological Bulletin found that specific feedback drives performance gains by focusing attention on the task, not the ego. In EMS/nursing, where split-second decisions matter, specificity ensures we’re tweaking the right skills—like nailing an airway instead of fumbling it. Without it, learners waste energy guessing what went wrong, and providers miss chances to refine their craft.
- EMS/Nursing Relevance: Our work is detail-oriented. A vague “good job” doesn’t tell a student why their patient rapport clicked or how to fix a sloppy splint. Specific feedback, like “Your history-taking caught the patient’s allergy, but you missed asking about recent falls,” guides precise growth. It’s the difference between a student who stalls and one who soars.
- Example: Instead of “Your intubation was off,” try, “You positioned the head well, but the laryngoscope angle was too shallow, making the cords hard to see.”
- Pitfall: Overloading with too many specifics can overwhelm. Focus on one or two key points per session, as per a 2020 study in Academic Medicine on cognitive load in feedback.
2. Timely: Striking While the Iron’s Hot
- What It Means: Timely feedback happens as close to the event as possible—ideally immediately for sims or within hours for real calls. It’s fresh, relevant, and memorable.
- Why It’s Critical: Feedback loses potency over time, like a 12-lead missing a STEMI. A 2020 study in Journal of Nursing Education found that immediate feedback in simulation training boosts skill retention by 30%. In EMS/nursing, where we’re juggling back-to-back calls or classes, timely feedback ensures the context is still vivid—whether it’s a botched IO or a stellar code. It also shows you care enough to address it now, not six months later at an eval. Delayed feedback risks fading details, leaving receivers disconnected from the lesson and less motivated to act.
- EMS/Nursing Relevance: Our fast-paced world demands quick feedback loops. A student who fumbles a trauma assessment in a sim needs input right after, not next week when they’ve forgotten the scenario. On real calls, a quick post-shift chat keeps it fresh without disrupting patient care. Timely feedback fuels the rapid learning curve we need to handle emergencies with confidence.
- Example: Post-sim, say, “Your compressions were spot-on, but let’s work on starting the code faster—aim for under 30 seconds next time.” Waiting a week dilutes the lesson.
- Pitfall: Timing feedback during high-stress moments (e.g., mid-code) can backfire. If emotions are raw, delay to post-shift or a private debrief, per a 2021 study in Simulation in Healthcare.
3. Actionable: The Roadmap to Growth
- What It Means: Actionable feedback provides a clear, obtainable goal or next step. Instead of “Work on your IVs,” say, “Try stabilizing the vein with your thumb to reduce rolling—let’s practice three sticks this week.”
- Why It’s Critical: Feedback without a plan is like handing someone a map with no destination. Actionable feedback gives receivers a concrete way to improve, boosting confidence and motivation. Hattie’s 2007 study emphasizes that feedback tied to clear goals fosters self-regulated learning, helping learners take ownership. In EMS/nursing, where we’re constantly upskilling, actionable feedback turns critiques into opportunities—like turning a shaky intubation into a slick one. Without actionability, feedback feels like a dead end, leaving receivers frustrated and stagnant.
- EMS/Nursing Relevance: Our field thrives on practical solutions. A student struggling with patient assessments needs a goal like “Practice the OPQRST method on five patients this shift.” A provider who fumbles a med dose needs a plan like “Double-check calculations with a partner for the next three calls.” Actionable feedback keeps growth within reach, ensuring we’re ready for the next call or code.
- Example: Instead of “You need better teamwork,” try, “You did great updating the team, but try assigning roles at the start of the code. Let’s run a sim tomorrow to practice.”
- Pitfall: Setting unrealistic goals (e.g., “Master intubation by tomorrow”) breeds frustration. Use S.M.A.R.T. goals (Specific, Measurable, Achievable, Relevant, Time-bound), per a 2019 study in Nurse Education Today.
4. Respectful: The Heart of Trust
- What It Means: Respectful feedback is delivered with kindness, humility, and positivity, even when critiquing. Start with a strength, frame critiques as opportunities, and avoid condescension.
- Why It’s Critical: Nobody grows when they feel attacked. A 2018 study in Academic Medicine found that respectful feedback reduces defensiveness and fosters a growth mindset. In EMS/nursing, where stress is high and egos can bruise, respectful feedback builds trust—whether it’s a student learning or a provider in the heat of a call. It’s about saying, “We’re in this together,” not “I’m better than you.” Disrespectful feedback shuts down learning, erodes team cohesion, and risks burnout in our already intense field.
- EMS/Nursing Relevance: Our culture values teamwork and resilience. A student who feels respected is more likely to ask questions and take risks, like practicing a new skill. A provider who’s critiqued kindly will trust their partner on the next call, not resent them. Respect turns feedback into a gift, not a gut-punch, fostering the camaraderie we need to thrive.
- Example: Instead of “You’re too slow,” say, “Your patient rapport was awesome, which calmed them down. Let’s work on pacing the assessment to under five minutes—great foundation to build on!”
- Pitfall: Overdoing praise can dilute the critique, making it feel insincere. Balance positives with honest, constructive input, as per a 2022 study in Journal of Clinical Nursing.
Where and When to Give Feedback: Timing and Location Deep Dive
Feedback’s impact hinges on where and when it’s delivered. Get this wrong, and even S.T.A.R. feedback can flop. Here’s a deeper look, with adjustments for context and evidence to back it up.
Timing
- Immediate (Post-Event): Best for training scenarios or low-stakes settings. A 2021 study in Simulation in Healthcare found immediate debriefs after sims improve performance by 20%. Example: Post-cardiac arrest sim, say, “Your compressions hit the mark; let’s practice faster defib prep.”
- Why It Works: Fresh context maximizes recall and relevance.
- Adjustment: If the receiver’s stressed, soften the tone and focus on one key point to avoid overload. Use more positives to keep morale high.
- EMS/Nursing Fit: Perfect for sim labs or post-drill debriefs, where students expect rapid input.
- Delayed (Same Day/Shift): Ideal for real-world calls or sensitive feedback. Waiting a few hours lets emotions settle but keeps it relevant. A 2020 study in Academic Medicine suggests a short delay reduces defensiveness.
- Why It Works: Gives time to reflect, ensuring a calmer discussion.
- Adjustment: Reference the event clearly (e.g., “On that trauma call this morning…”). Pair with a specific goal to keep it forward-looking.
- EMS/Nursing Fit: Great for post-shift chats in the ambulance bay or ED break room, after the chaos subsides.
- Scheduled (Weekly/Monthly): Best for big-picture feedback, like tracking progress toward long-term goals. A 2019 study in Nurse Education Today found regular check-ins boost student confidence by 15%.
- Why It Works: Allows comprehensive discussion and goal-setting.
- Adjustment: Use a structured format (e.g., review specific incidents, set S.M.A.R.T. goals). Encourage two-way dialogue to keep it collaborative.
- EMS/Nursing Fit: Perfect for precepting meetings or educator-student check-ins, where you can map out skill development.
Location
- Private Setting (Office, Break Room): The gold standard for constructive or sensitive feedback. A 2022 study in Journal of Clinical Nursing found private feedback preserves dignity and fosters openness.
- When: Post-shift, during a debrief, or in a scheduled meeting.
- Example: Pull a student into a quiet office to discuss pacing issues after a sim.
- Adjustment: Use full S.T.A.R. with detailed examples and goals. Ensure a distraction-free space to encourage dialogue.
- EMS/Nursing Fit: Ideal for addressing skill gaps or sensitive topics, like a provider’s hesitation during a code.
- Semi-Private (Sideline of a Sim/Call): Works for quick, low-stakes feedback during training. Keep it brief and positive-leaning to avoid embarrassment.
- When: Mid-sim or post-call, away from patients or crowds.
- Example: Whisper to a provider, “Great airway management; try tilting the head more next time.”
- Adjustment: Shorten S.T.A.R. to specific-actionable points. Save deeper critique for private settings.
- EMS/Nursing Fit: Useful in sim labs or during downtime on a call, when immediate tweaks can enhance performance.
- Public (In Front of Others): Only for praise, unless it’s a group debrief where critique is expected. A 2018 study in Medical Education warns that public criticism tanks morale.
- When: For positive reinforcement, like, “Awesome teamwork on that code, everyone!”
- Example: Congratulate a student in front of the class for a stellar assessment.
- Adjustment: Keep it brief, positive, and group-focused to boost morale. Avoid singling out for critique.
- EMS/Nursing Fit: Great for boosting team spirit in class or after a successful call.
Adjusting Based on Context
- High-Stress Moments: After a tough call, delay feedback until emotions cool (e.g., end of shift). Use extra respect and empathy, starting with a strong positive to ease tension.
- Training vs. Real World: Sims allow immediate, detailed feedback; real calls need delayed, private delivery to avoid undermining confidence in front of patients.
- Cultural/Personality Differences: Some prefer directness; others need more positives. A 2020 study in Academic Medicine suggests asking, “How do you like feedback?” to tailor your approach.
- Group vs. Individual: In group debriefs, generalize critique (e.g., “Let’s all work on faster role assignment”) and save individual feedback for private moments.
Feedback in Action: Good vs. Bad Examples
Let’s see S.T.A.R. in action across our three dynamics, with good and bad examples to highlight what works and what crashes.
Teacher to Student
- Scenario: Student Sarah struggles with an intubation sim.
- Bad Example (Public, Vague, Disrespectful):
- Where/When: In the sim lab, in front of peers, mid-scenario.
- Feedback: “Sarah, you’re nowhere near ready for intubation. That was a mess.”
- Why It Fails: Public shaming kills confidence. It’s vague (no specific critique) and offers no path forward, violating Academic Medicine (2018) on fostering growth.
- Good Example (Private, S.T.A.R.):
- Where/When: In a quiet corner of the sim lab, post-scenario.
- Feedback: “Sarah, your prep for the intubation was thorough, which set a great tone (specific, respectful). The tube took a bit because the laryngoscope angle was off, blocking the cords (specific, timely). Try tilting the blade 10 degrees more—let’s practice three times this week in the lab (actionable). You’re building solid skills, so keep at it (respectful).”
- Why It Works: Private setting preserves dignity. S.T.A.R. provides clarity and a goal, aligning with Wisniewski et al. (2019).
Student to Teacher
- Scenario: Sarah finds my trauma lecture confusing.
- Bad Example (Public, Vague):
- Where/When: In class, blurted out during a lecture.
- Feedback: “Jake, this trauma stuff is a mess. Can you teach better?”
- Why It Fails: Public delivery embarrasses the instructor and peers. It’s vague and non-actionable, ignoring S.T.A.R. principles.
- Good Example (Private, S.T.A.R.):
- Where/When: In my office, after class.
- Feedback: “Jake, your real-world stories make trauma relatable, which helps a ton (specific, respectful). The triage section felt rushed today, and I got lost (specific, timely). Could we slow down on triage steps and add a practice scenario next class? (actionable). Your passion keeps us engaged, so thanks (respectful).”
- Why It Works: Private setting fosters trust. S.T.A.R. gives clear, actionable input, per Hattie (2007).
Provider to Provider
- Scenario: Nurse Mike and I fumble an IO placement during a trauma call.
- Bad Example (Semi-Public, Harsh):
- Where/When: In the ED trauma bay, mid-call, near staff.
- Feedback: “Mike, you botched that IO. Get it together.”
- Why It Fails: Semi-public critique undermines teamwork. It’s vague and disrespectful, ignoring Journal of Clinical Nursing (2022) on dignity.
- Good Example (Private, S.T.A.R.):
- Where/When: In the break room, post-shift.
- Feedback: “Mike, your triage kept that trauma call organized—clutch move (specific, respectful). The IO took a bit because we didn’t stabilize the drill well (specific, timely). Let’s run a 15-minute IO drill tomorrow to hit under 30 seconds (actionable). You’re a rockstar under pressure (respectful).”
- Why It Works: Private setting builds trust. S.T.A.R. offers a clear plan, per Kluger and DeNisi (1996).
New Ideas: Tech and AI to Supercharge Feedback
Let’s push the envelope with feedback in EMS and nursing. Here are two fresh ideas, rooted in research and tailored for our field:
- AI-Driven Feedback Dashboard: Imagine a sim platform with AI tracking metrics like compression rate, decision speed, and teamwork dynamics. Post-sim, it generates a S.T.A.R. report: “Your airway management was 95% effective (specific). You paused 8 seconds before defib (timely). Practice charging in under 5 seconds (actionable). Strong leadership noted (respectful).” A 2021 study in Medical Teacher by Chan et al. shows AI delivers objective, bias-free feedback.
- Timing/Location: Use in private debriefs or scheduled reviews to avoid public overwhelm. Immediate for sims, delayed for real calls.
- EMS/Nursing Fit: Perfect for sim labs, where data-driven input complements human feedback.
- Feedback App with Goal Tracking: Create a mobile app where students and providers log feedback, set S.M.A.R.T. goals, and track progress. Example: After I critique Sarah’s intubation, she logs it, sets a goal to nail three tubes by week’s end, and checks in via the app. A 2022 study in Nurse Education Today found digital reflection tools boost self-awareness by 20%.
- Timing/Location: Log feedback privately post-session. Review goals in scheduled check-ins for deeper discussion.
- EMS/Nursing Fit: Ideal for busy providers juggling shifts and students tracking precepting goals.
Pitfalls to Avoid: Don’t Be That Medic
Feedback can go south fast. Here are common EMS/nursing fails and how to sidestep them:
- Public Shaming: Critiquing in front of patients or peers kills morale. Always go private for constructive feedback.
- Vague Vibes: “Do better” is as useful as a broken stethoscope. Use S.T.A.R. for clarity.
- Ego Overload: Feedback isn’t your chance to flex. Stay humble—admit when you’ve learned something too.
- No Follow-Up: Don’t drop feedback and ghost. Check in on goals, especially in scheduled reviews.
- Wrong Timing/Place: Yelling critique mid-call or in a busy ED is a recipe for resentment. Wait for a private, calm moment.
Wrapping It Up: Feedback as a Lifeline
Feedback in EMS and nursing is like a well-timed defibrillation—it shocks us into better performance. Whether you’re a teacher shaping a student, a student guiding your instructor, or a provider lifting a colleague, feedback builds skills, trust, and teamwork. Use the S.T.A.R. method to keep it specific, timely, actionable, and respectful. Pick the right time and place—immediate for sims, delayed for real calls, private for critique, public for praise. Adjust your approach based on context, stress levels, and personalities. Embrace tech like AI dashboards or feedback apps to make it smarter. And always deliver with humility and a chuckle—because we’re all human, even the paramedic who swears that coffee lid was secure.
So, go give feedback that sticks, grows, and saves lives. And maybe invest in a spill-proof mug while you’re at it.
Click each image to download a PDF Version
References:
- Wisniewski, B., et al. (2019). Effective feedback in clinical education: A meta-analysis. Medical Education, 53(10), 949–961.
- Hattie, J., & Timperley, H. (2007). The power of feedback. Review of Educational Research, 77(1), 81–112.
- Kluger, A. N., & DeNisi, A. (1996). The effects of feedback interventions on performance. Psychological Bulletin, 119(2), 254–284.
- Chan, K. S., et al. (2021). Artificial intelligence in medical education: Opportunities and challenges. Medical Teacher, 43(3), 302–309.
- Smith, L., et al. (2022). Reflective journaling in nursing education: A tool for self-regulated learning. Nurse Education Today, 108, 105–112.
- Johnson, C., et al. (2021). The impact of immediate feedback in simulation-based training. Simulation in Healthcare, 16(4), 245–252.
- Brown, T., et al. (2020). Tailoring feedback to learner preferences. Academic Medicine, 95(6), 876–882.