Let me paint you a picture.
Almost 20 years deep into EMS life, thinking I’m finally getting a handle on those little ECG squiggles—and then boom. I stumble across something that makes me feel like a total genius and a complete rookie in the same moment. Enter: the precordial swirl.
Never heard of it? Me neither, until a recent research article came out!
Let’s talk about it. Because this sneaky little pattern has been hiding right in front of us—and we’ve probably missed more than a few ticking LAD time bombs because of it.
What the Heck Is a Precordial Swirl?
Okay, imagine this.
You’re looking at an ECG—not one of those dramatic, text-your-medical-director kind of ECGs, but something a little… off. The kind where you squint and mutter, “Hmm, that’s weird” before moving on because you’re not entirely sure what’s bothering you.
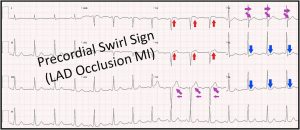
Turns out, when the left anterior descending artery (LAD) decides to check out (specifically the proximal part), the ECG doesn’t always give you your classic, bold ST elevations in V2-V4.
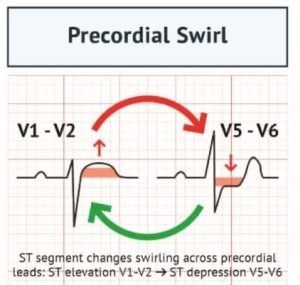
Instead, it does something different—like a little electrical tornado across the precordial leads. Here’s how it breaks down:
V1–V2: Inappropriate ST elevation and/or hyperacute T waves (basically, stuff that shouldn’t be there)
V5–V6: Reciprocal ST depression and/or inverted T waves
So what you end up with is this clockwise swirl—like the heart’s having a subtle, deadly dance party across the chest leads.
And no, this isn’t just ECG poetry. It’s backed by research. Real-deal, peer-reviewed, life-saving stuff.
The Numbers (Brace Yourself)
A group of clever researchers studied 808 high-risk patients—you know, the ones who look like they’re seconds from coding in the back of your rig—and found this pattern lurking in some of the most critical ones.
Here’s what they found:
Specificity: 92–98%
Sensitivity: 9–11% (yes, that’s low—but hang on)
Positive Predictive Value: 42–70%
Now before you scoff at that sad little sensitivity number, remember: This isn’t about catching every heart attack. It’s about catching the ones that slip right past our current STEMI criteria. You know the ones—those “NSTEMIs” that get a nice bed on the telemetry floor while their LAD quietly dies.
Get this: 70% of the patients with the precordial swirl pattern were missed by traditional STEMI criteria.
Let that sink in. Seven out of ten.
So, Uh… Why Does This Happen?
Alright, it’s time for the obligatory geek-out section. I’ll try not to sound too smug, but fair warning—I just had my second coffee and I’m feeling bold.
When the LAD gets blocked—specifically proximal to the first septal perforator—it sets off a chain reaction that messes with the heart’s electrical mojo.
V1 and V2 sit right over the septum and right ventricle.
When the anterior septum starts starving for oxygen, those leads pick up the distress signals.
Boom: ST elevation and hyperacute T waves in V1–V2.
Meanwhile…
V5 and V6 are over the lateral wall of the left ventricle.
That part of the heart isn’t happy either, and it starts throwing inverse changes—ST depression and T-wave inversions.
The result? A weird, swirling electrical pattern that mimics a tornado across the chest leads. It’s like the heart is waving a little flag, going, “Hey… things are bad up here,” and we just shrug because the ST elevation isn’t where we expect it to be.
Why This Matters (a.k.a. My Moment of Shame)
Here’s the painful truth: I’ve definitely missed this before.
Like… definitely.
I’ve probably seen this pattern and filed it away as “non-specific changes” while sending the patient upstairs with some aspirin and a shrug. But now? I’m kicking myself. Hard.
This pattern shows up when the LAD occludes just right—or maybe just wrong—in a spot that causes serious damage without triggering the big flashy ECG red flags we’re taught to look for.
It’s like the heart attack equivalent of a stealth bomber: invisible to radar until it’s way too late.
But Wait—There’s a Catch (Of Course There Is)
Before you start diagnosing every off-looking ECG as a precordial swirl, take a breath. A few deep ones, actually.
This pattern has some very convincing mimics, including:
Left Ventricular Hypertrophy (LVH) – loves messing with repolarization
Diffuse subendocardial ischemia – loves messing with everything
Bundle Branch Blocks – those big ol’ wide QRS complexes throw everything off
Ventricular Paced Rhythms – good luck interpreting anything here
The swirl is only valid in normal, narrow QRS complexes. If your QRS is wide, if there’s evidence of LVH, or if your patient’s being paced—don’t go chasing swirls.
What This Means for Us Street Dogs
Let’s be real: the precordial swirl isn’t going to get its own line in your protocol anytime soon. But it should get a spot in your brain right next to “gut feeling” and “something ain’t right.”
Here’s what this pattern is telling us:
Our current STEMI criteria are missing people—like, a lot of them.
This swirl may be subtle, but it’s real. When it shows up, it often means a proximal LAD is occluded.
You don’t need to be a cardiologist. Just trust your instincts and take a second look when things feel off.
If your patient looks like garbage but their ECG looks almost normal? Zoom in on those V1–V2 and V5–V6 leads. They might be doing the swirl.
And if they are—call it. Don’t wait.
Bottom Line (If You Skimmed to Here, I Get It)
Pattern Recognition:
V1–V2: inappropriate ST elevation or hyperacute T waves
V5–V6: reciprocal ST depression or inverted T waves
Normal QRS complex is a must
Clinical Significance:
92–98% specificity for LAD occlusion
70% of swirl patients were missed by standard STEMI rules
Usually indicates proximal LAD involvement
Low sensitivity = not for every MI, but great for hidden ones
Common Mimics (Be Cautious):
LVH
Diffuse ischemia
Bundle branch blocks
Paced rhythms
Takeaway for Field Providers:
Don’t toss out an ECG just because it’s not textbook
Trust the story the patient is telling you
If you see this pattern and your gut says “not right,” speak up
Powerful Medical 20. April 2025
Powerful Medical 20. April 2025
Final Thoughts (From One Medic to Another)
I’ll be honest. Reading about this pattern made me both excited and annoyed. Excited that I learned something that could actually help patients. Annoyed that I probably missed it five times last year alone.
But hey—that’s medicine. It’s humbling. Just when you think you’ve seen it all, the heart throws you a curveball shaped like a swirl.
So next time you’re looking at an ECG that just feels off—especially in a patient with chest pain—zoom in on V1–V2 and V5–V6. Look for the swirl.
And if you see it? You might’ve just caught the MI that everyone else missed.
Now go forth, swirl-spotter. Impress your colleagues. Save a heart.
Just… maybe don’t let it go to your head. We’ve all still got a lot to learn.
Reference:
Goss L, Meyers HP, Friedman B, Bracey A, Smith SW. Precordial swirl sign: A new ECG pattern of left anterior descending artery occlusion myocardial infarction. Journal of Electrocardiology. 2025. https://doi.org/10.1016/j.jelectrocard.2025.153931
P.S. If you really want to lose sleep, go read Dr. Smith’s ECG blog. It’ll make you question everything you thought you knew about anterior ischemia. In the best way.
P.P.S. One time I accidentally diagnosed SVT on a patient with a slightly bouncy ambulance monitor cable. True story. Stay humble.