Every now and then, some research paper comes along that makes me pause, sip my coffee, and say, “Well, that explains why the last time I tried that, it didn’t work the way I thought.” This one, published in Critical Care Medicine in 2023, digs into something we’ve all done at one point or another; clamping an endotracheal tube.
You know the drill. You’re changing out a ventilator circuit, swapping filters, or moving a patient, and you want to keep their lungs from deflating like a dollar-store balloon at a kid’s birthday party. The solution? Clamp the tube. Simple, right? Well, not so fast. Turns out not all clamps, timings, or tube sizes are created equal.
Why We Clamp in the First Place
Before we get lost in the weeds of which clamp beats which, let’s answer the big “why.” Why would anyone want to squeeze off a patient’s lifeline of air?
Preventing the Big Whoosh
You know that awful sound when a vent circuit pops off mid-transport? The patient’s lungs just dump everything in one ugly rush. A clamp stops that whoosh, keeps alveoli open, and buys you time.Aspiration Insurance
Switching circuits or bagging during transport basically leaves the airway wide open for junk to slide in. Clamping is like shutting the garage door before the dust storm rolls through.Keeping PEEP Where It Belongs
Positive End-Expiratory Pressure (PEEP) is the secret sauce that keeps alveoli from collapsing. Disconnect without clamping, and poof — it’s gone. Clamp first, and you protect that pressure like a bodyguard at the lung nightclub.High-Stakes Moves (like ECMO or long transports)
When your patient’s life depends on rock-solid airway pressure, clamping before disconnect is the difference between smooth sailing and a crash course in lung recruitment you really didn’t want.
Bottom line — clamping isn’t about being fancy. It’s about controlling chaos, preventing setbacks, and making sure the patient doesn’t lose ground while you’re trying to help them.
The Experiment in a Nutshell
The researchers tested three different clamps:
Klemmer forceps (your basic OR-style metal tool)
Chest-tube clamp (big, plastic, kind of clunky)
ECMO clamp (the heavy-duty big brother built for serious tubing)
They tried these out on simulated lungs with ETTs sized 6, 7, and 8 mm. They clamped at different points in the breathing cycle:
End of exhalation
End of inhalation
End of inhalation, but with the tidal volume cut in half
Then they left the lung “clamped” for 5, 15, and 30 seconds, disconnected from the vent, and checked what happened to airway pressure and lung volume.
What They Found (Without the Nerd Speak)
Clamp choice matters.
On a small tube (6 mm), most clamps worked okay. But on 7–8 mm tubes, the ECMO clamp was the only one that really did its job. The others were kind of “meh.”Timing matters even more.
Best results came from clamping at the end of inhalation. Clamping at the end of exhalation just didn’t hold pressures well.Beware the garden-hose effect.
Clamping at full inspiration held volume, but reconnecting caused nasty pressure spikes — like holding your thumb over a garden hose and then letting go. The best move? Clamp at inspiration but cut the tidal volume in half first. Holds steady, reconnects smooth.
The Big Takeaways
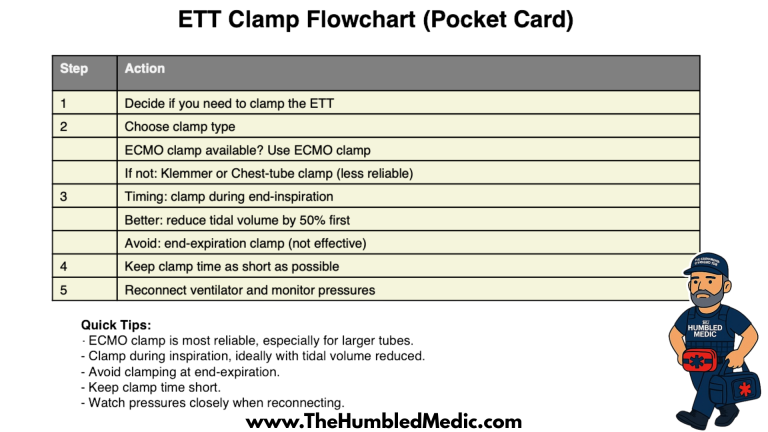
Here’s the cheat sheet:
If you’ve got an ECMO clamp, use it. It’s the muscle car of clamps.
Clamp during inspiration, but don’t max out the lungs. Half a breath is your friend.
Don’t bother clamping at the end of exhalation — it doesn’t hold.
Keep clamp time short. Every second clamped is a gamble.
The Real-World Paramedic Perspective
Now, before you start rolling your eyes at the idea of fancy clamps, let me say this: go bug your supply officer. Seriously. If the research tells us ECMO clamps are the clear winners, then why wouldn’t we want the right tool for the job on our rigs? We carry all sorts of expensive gear we might only use once in a blue moon — why not something that can literally protect a patient’s lungs in seconds? This isn’t about being bougie, it’s about being prepared.
And here’s a little friendly reminder from the school of hard knocks: make sure you’re actually grabbing a clamp. Not scissors. Not trauma shears. A clamp. I wish I was joking, but it’s happened. Nothing wakes you up quite like realizing you’ve just snipped through your patient’s ET Tube when you meant to pinch it shut. So yeah, ECMO clamps in the bag, and maybe a little double-check before you squeeze.
For me, the biggest win from this study is still the tidal volume trick. Half a breath before clamping keeps the pressures smooth on reconnect. Combine that with the right clamp, and you’re setting your patient up for success instead of extra problems.
Bottom Line
Clamping can be a lifesaver, but like everything else in critical care, it’s not just about doing the thing. It’s about doing it right. Use the right clamp, at the right time, for the right reason.
Think of it this way, clamping the tube isn’t about showing off your tools. It’s about protecting your patient from chaos. And if you do it right, you’ll keep the lungs inflated, the PEEP where it belongs, and maybe even keep your partner from giving you the side-eye when the vent circuit goes flying.
Sometimes, the simplest tools, used smartly, make all the difference.
References
Ferré A, Wallet F, Vallée F, et al. Efficacy of Different Clamps and Strategies for Endotracheal Tube Clamping: A Bench Study. Critical Care Medicine. 2023;51(9):1351-1359. doi:10.1097/CCM.0000000000005964
POCKET CARD