Ever been on a long road trip where every exit looks the same, and you’re not sure which one leads to food, fuel, or that sketchy gas station burrito you’ll regret later? Welcome to the nephron! A winding highway through the kidney where each “exit” has a different purpose. The body pulls off sodium, water, electrolytes, and acids like pit stops along the way.
Diuretics are like traffic cops with cones and flashing lights, blocking lanes and forcing detours. If you know which exit each drug works on, you’ll predict what’s coming: the urine volume, the electrolyte fallout, and the side effects.
Let’s hit the road.
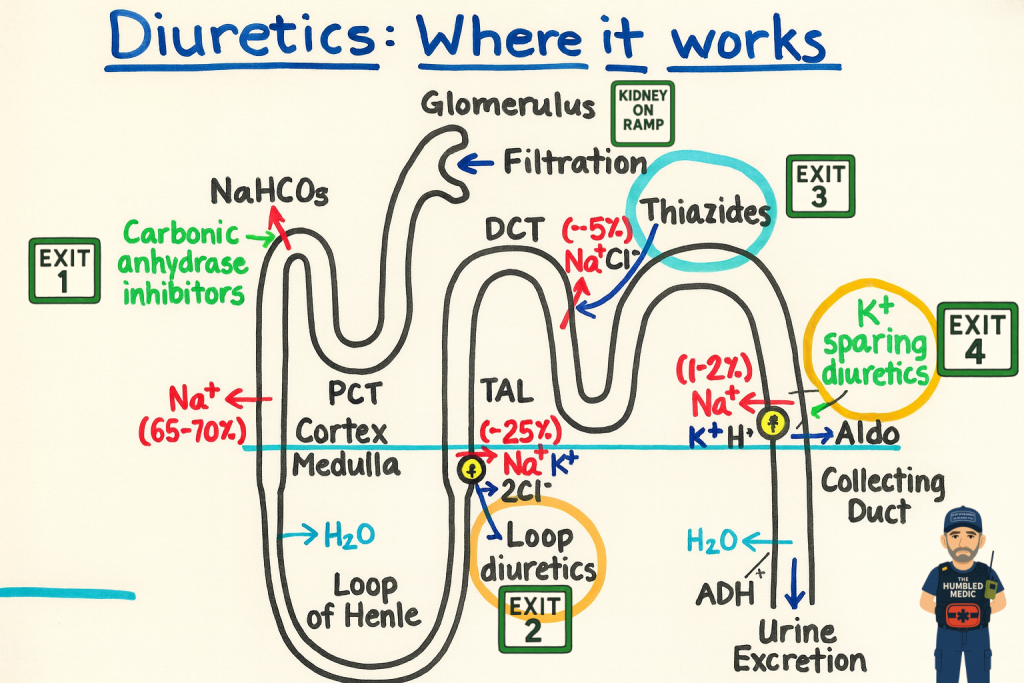
🚦 The Glomerulus Toll Booth (Filtration)
This is the on-ramp. Everything small enough — sodium, water, glucose, chloride, bicarbonate, pays the toll and enters the nephron. Large stuff like proteins and cells stay behind.
Patho Deep Dive: Filtration depends on blood pressure, oncotic pressure, and the health of the glomerulus. Mess with any of those and traffic slows down before the first exit.
🚧 Exit 1: Proximal Tubule (Carbonic Anhydrase Inhibitors)
Here’s the first rest stop, where 65–70% of sodium and water normally get reabsorbed along with bicarbonate.
Medications: Acetazolamide, Methazolamide
How they work: They block the enzyme carbonic anhydrase, so less sodium bicarbonate gets reabsorbed. Sodium, bicarbonate, and water are excreted.
Why it matters: These aren’t everyday workhorses; think altitude sickness, metabolic alkalosis, or systemic glaucoma treatment.
Risks: Metabolic acidosis, hypokalemia, kidney stones.
Patho angle: Blocking bicarbonate reabsorption makes the blood more acidic. In altitude sickness, that acidosis actually helps you breathe better by stimulating ventilation.
🌀 Exit 2: Loop of Henle (Loop Diuretics)
Now we’re on the big bend of the highway. Here, about 25% of sodium is reabsorbed. Loop diuretics slam the brakes on the Na⁺/K⁺/2Cl⁻ pump.
Medications: Furosemide, Torsemide, Bumetanide, Ethacrynic acid
Effect: Sodium, chloride, potassium, calcium, and magnesium all get excreted, with a large amount of water following.
Uses: Pulmonary edema, CHF, renal failure, hypercalcemia.
Risks: Hypokalemia, hypomagnesemia, metabolic alkalosis, ototoxicity.
Patho angle: Because calcium and magnesium hitch a ride with sodium reabsorption, loops cut those off too. That’s why loop diuretics are your go-to when calcium is dangerously high.
🛣 Exit 3: Distal Convoluted Tubule (Thiazides)
This exit is more like a side street. Only about 5% of sodium is reabsorbed here, but it matters for long-term traffic control.
Medications: Hydrochlorothiazide, Chlorthalidone, Metolazone, Indapamide
Effect: Blocks the sodium-chloride symporter, causing mild diuresis while increasing calcium reabsorption.
Uses: Hypertension, prevention of kidney stones, CHF adjunct.
Risks: Hyponatremia, hypokalemia, increased uric acid and glucose, hypercalcemia.
Patho angle: The calcium effect is unique — unlike loops, thiazides help retain calcium. That’s why patients with recurrent calcium stones sometimes get thiazides prescribed.
🛑 Exit 4: Collecting Duct (Potassium-Sparing Diuretics)
Here’s the toll booth where aldosterone calls the shots: sodium stays, potassium goes. Potassium-sparing diuretics flip that switch.
Medications: Spironolactone, Eplerenone, Amiloride, Triamterene
Effect: Retain potassium while excreting sodium.
Uses: CHF (spironolactone improves survival), cirrhosis ascites, resistant hypertension.
Risks: Hyperkalemia, gynecomastia (spironolactone).
Patho angle: Spironolactone isn’t fast — it needs aldosterone to be active to block it. That’s why it won’t bail you out in pulmonary edema today, but it’ll keep your CHF patient alive longer down the road.
🗺️ Roadmap Recap
Loops = Interstate closure → massive fluid dump
Thiazides = Side street detour → slow, steady pressure control
K⁺ sparers = Toll booth override → fine-tuning potassium balance
CAIs = Weird backroad → not for daily traffic, but sometimes critical
🚑 Why This Map Matters
In the field: Know that furosemide hits in minutes, while spironolactone takes days.
On the floor: Predict labs — thiazides raise calcium, loops lower it.
For patient safety: The roadmap lets you anticipate crashes before they happen.
When you look at the nephron like a highway, each drug’s job becomes crystal clear. And just like a road trip, knowing your exits ahead of time makes the ride a whole lot smoother.
Exit-by-Exit Medication Deep Dive
🚧 Exit 1: Carbonic Anhydrase Inhibitors
Meds: Acetazolamide, Methazolamide
Mechanism: Inhibit carbonic anhydrase → lose Na⁺ and HCO₃⁻ → metabolic acidosis
Pharmacokinetics: Onset 1–2 hrs PO; duration 8–12 hrs
Pearl: Rarely used for volume; mostly for niche indications
🌀 Exit 2: Loop Diuretics
Meds: Furosemide, Torsemide, Bumetanide, Ethacrynic acid
Mechanism: Block Na⁺/K⁺/2Cl⁻ pump → dump Na⁺, Cl⁻, K⁺, Ca²⁺, Mg²⁺, and water
Pharmacokinetics: IV furosemide onset 5 min; torsemide has a longer half-life
Pearl: Torsemide may outperform furosemide in CHF
🛣 Exit 3: Thiazides
Meds: Hydrochlorothiazide, Chlorthalidone, Metolazone, Indapamide
Mechanism: Block Na⁺/Cl⁻ pump; increase Ca²⁺ retention
Pharmacokinetics: Chlorthalidone lasts 24–72 hrs (longer than HCTZ)
Pearl: Metolazone + loop = powerful combo, but monitor closely
🛑 Exit 4: Potassium-Sparing Diuretics
Meds: Spironolactone, Eplerenone, Amiloride, Triamterene
Mechanism: Block aldosterone or sodium channels
Pharmacokinetics: Spironolactone onset 24–48 hrs
Pearl: Best used in combination with loops or thiazides
Loop Diuretics: The Big Guns
Loops are like pulling the fire alarm in the kidney. They work in the loop of Henle, and when they hit, everything comes rushing out—sodium, potassium, calcium, magnesium, water… you name it. If your patient’s drowning in fluid, loops will bail the boat out fast.
How I remember: Loops make you lose everything. Simple, but it sticks.
What to watch for?
Hypokalemia—that monitor might start spelling out arrhythmias if you’re not careful.
Hypomagnesemia and hypocalcemia—they’re losing more than just water.
Hyperuricemia—cue the gout flare.
In kids, they can even mess with kidney stones.
Pro tip from the field: never push furosemide before a long transport unless you want to play “find a bathroom” on wheels.
Thiazide Diuretics: The Slow Burn
Now, thiazides are like that coworker who just quietly gets the job done. They hang out in the distal tubules, gently letting sodium and water trickle away. Not as flashy as loops, but they’re perfect for steady blood pressure control.
Memory trick: Thia-ZIDE keeps you ZIDEd (sided) with steady control.
What to watch for?
Hypokalemia, hyponatremia, hypomagnesemia. Basically, electrolytes go sideways.
Hypercalcemia—unlike loops, thiazides actually hold onto calcium.
Can raise cholesterol, sugar, and uric acid. Basically, the lab panel starts looking like Thanksgiving leftovers.
Pro tip: these are great for blood pressure but useless if someone’s crashing with pulmonary edema. Don’t bring a garden hose to a house fire.
Potassium-Sparing Diuretics: The Gentle Touch
These guys work at the distal tubule and collecting duct, keeping potassium in the body while still moving out sodium and water. They’re not strong enough to headline a show, but they make great backup singers when paired with other diuretics.
How I remember: They spare the potassium, spare the cramps.
What to watch for?
Hyperkalemia—tall, pointy T-waves will show up on the monitor if you’re not watching.
Spironolactone can cause gynecomastia. Yep. That conversation never gets easier.
Pro tip: they’re slow-acting. If you’re expecting them to fix acute fluid overload, you’ll be waiting until the next shift comes in.
Where They Work: The Plumbing Analogy
Think of the nephron like a water park:
Loops = the giant water slide (massive whoosh of water out)
Thiazides = the lazy river (slow, steady, chill)
K+ Sparers = the lifeguards (they keep potassium from sneaking out of the pool)
Monitoring: The Basics We Can’t Ignore
Every diuretic comes with a catch, so keep an eye on:
Electrolytes (especially potassium, sodium, and calcium)
Renal function (bad kidneys = bad news)
Blood pressure (don’t trade fluid overload for shock)
Daily weights (seriously, these tell you more than a foley bag ever will)
My Medic Memory Tricks
Loops Lose it all
Thiazides Trick sodium, keep calcium
K-sparers Spare potassium
Speed: loops = fast, thiazides = medium, K-sparers = slow
🛑 Final Rest Stop
At the end of the day, diuretics are just roadblocks we place along the kidney’s highway. Where they set up shop tells you everything about what’s going to happen downstream. Loops flood the road, thiazides detour the flow, and K-sparers guard potassium at the toll booth.
And here’s the thing: once you know the roadmap, you stop memorizing random side effects and start understanding them. That’s the difference between rattling off facts and actually practicing like the seasoned medic or nurse your patients need.
📚 References
Katzung BG, Vanderah TW. Basic and Clinical Pharmacology. 16th ed. McGraw-Hill Education; 2021.
Bledsoe BE, Porter RS, Cherry RA. Paramedic Care: Principles & Practice. 6th ed. Pearson Education; 2022.
Marino PL. The ICU Book. 4th ed. Lippincott Williams & Wilkins; 2014.
Porth CM. Essentials of Pathophysiology. 5th ed. Wolters Kluwer; 2022.
Prehospital Emergency Pharmacology. 8th ed. Pearson Education; 2021.